What’s in this article?
The True Cost of Fertility
The Family-Building Revolution
Falling through the NHS net
Navigating the private sector
Where do we go from here?
About Fertility Mapper
Contact Information
This report explores private and NHS access to fertility treatments in the UK, and aims to shed light on the complexity faced by fertility patients when navigating their treatment journeys.
If you'd like to read more about how to budget for your treatment, we've developed handy guides which break down the cost of IVF and Egg Freezing, and list the financing options available to you, including NHS funding. To find out whether you're eligible for NHS-funded IVF in seconds, check out our new NHS IVF Eligibility Calculator.
Forward
Kayleigh Hartigan, Founder and CEO - Fertility Mapper
I first started to think about the idea that would become Fertility Mapper years ago, when I moved from working in NHS management into private equity advisory. My experience provided perspective across both spheres of healthcare, and I saw just how much private money was shaping the healthcare market.
Perhaps nowhere is this more true than the fertility sector. While there is access to fertility treatment on the NHS, the sector is predominantly a private one. Fertility is not simply a question of "sickness" in the traditional sense - it's also about the choices we make in deciding when, and how, we start our families. Those choices are rapidly evolving: from deciding to start families later in life, to incorporating non-nuclear, non-heteronormative models of what a family looks like. And that means that more of us than ever before need, and rely on, fertility services to start our families.
The result? A booming private fertility market worth $21.13bn globally - and growing.
The boom has a darker side. Because if you need fertility services and support, then you face what can quickly become one of the most confusing, difficult and lonely experiences of your life.
At a time when you are vulnerable emotionally and physically, you will need to take some of the most expensive and life-altering decisions you will ever make - using information that's fragmented, difficult to understand and in some cases, plain misleading. From learning to navigate complicated NHS eligibility criteria, to finding yourself needing private treatment perhaps for the very first time, the experience for far too many people is simply unacceptable.
I founded Fertility Mapper in the firm belief that people deserve better. Getting fertility treatment should be easier, and far simpler. In order to drive real change, you first have to understand the full scope of the problem.
And that's what The True Cost of Fertility report is all about.
Drawing upon our own in-depth research and the data we have gained from hundreds of user reviews, we have created a much-needed 'whole picture' view that brings together data from across both the NHS and the private spheres of the fertility sector.
By sharing it with you, we hope to raise awareness and understanding of the true cost of fertility in the UK.
The True Cost of Fertility
At Fertility Mapper, we know there is so much more to the challenges facing the fertility sector than cost alone. But we believe, when it comes to empowering people, transparency around cost is a key first step in the fight to create fairer access to high quality fertility services.
As demand for fertility treatment, support and preservation grows, current research and information treats the NHS and the private sector as separate markets. But for people trying to access fertility treatment, there isn't a distinction. The restrictions of NHS-funded fertility services means more and more families move into private routes - and both sectors are characterised by a lack of clarity and transparency.
The True Cost of Fertility takes a cross-sector approach to looking at the problem. We consider the issue of cost from two perspectives that are often treated separately, but which for many people, are actually interlinked:
- what the NHS does (and does not) fund;
- what people pay privately for.
Our aim is to raise awareness of these two factors, and uncover the truth of the cost of fertility in the UK.
Key Findings
Complexity hides a multitude of sins across the sector that seriously impacts people's access to, and experience of, fertility treatment.
- NHS-funded fertility treatment is more than just a postcode lottery - it's a personal lottery, too: in eligibility, in wait times, and in generosity of offer:
- Almost half (46%) of regional NHS boards in England will only offer IVF if the maternal partner is aged under 40 and one ICB will only offer IVF if she is under 35.
- Three-quarters (76%) of ICBs won't fund IVF if either partner has any living children - even if they're from previous relationships.
- Many private clinics don't include key components of fertility treatment in their advertised package prices, and what's included and not included varies widely between clinics. This means that treatment often costs more than initially sold, and it's impossible to accurately choose a clinic based on price:
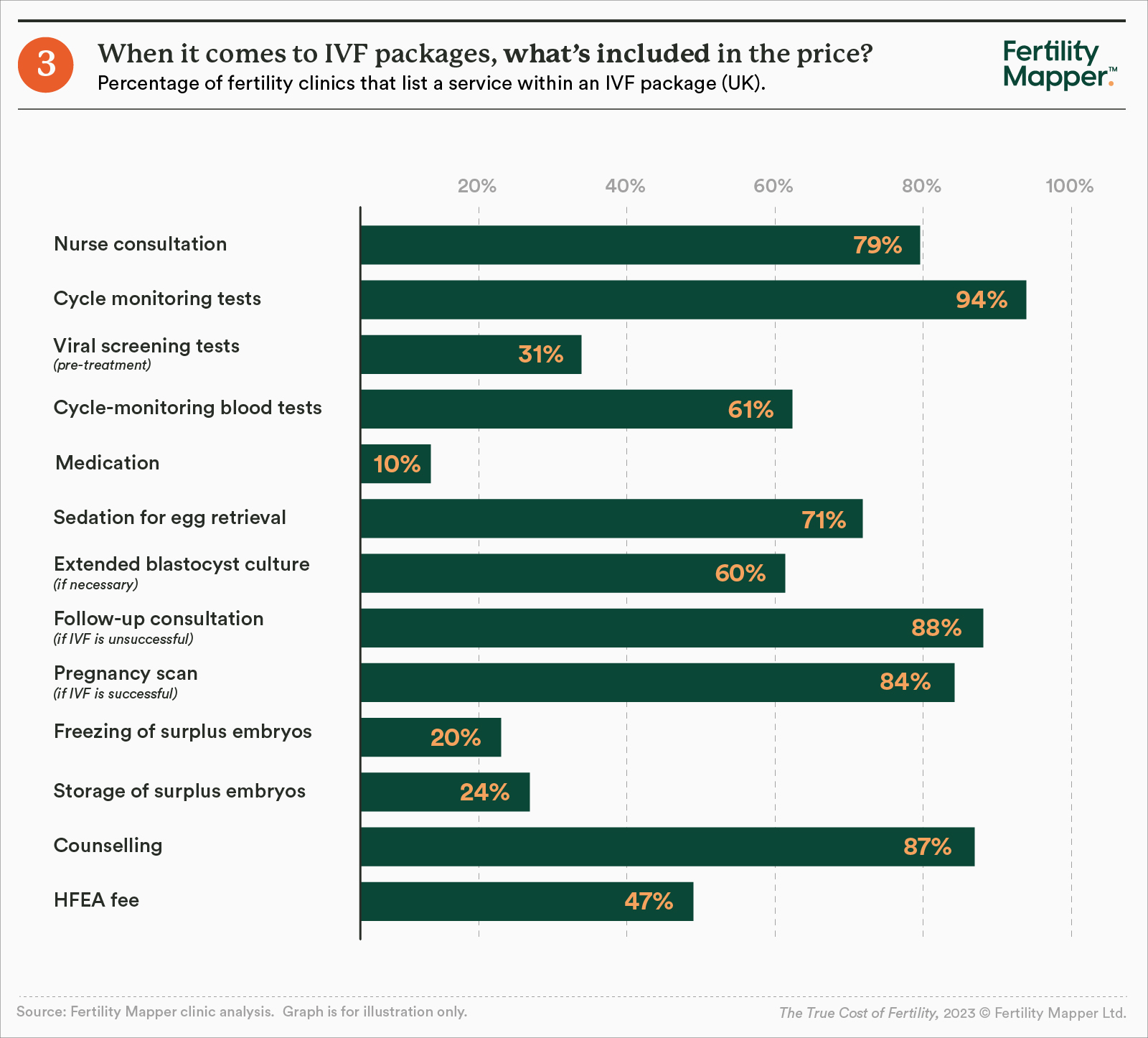
- Only 61% of clinics include blood tests in the advertised price of their IVF package, while only 31% include HFEA-mandated viral screening, and 24% include storage of surplus embryos.
- At a quarter of the clinics we measured, a standard course of IVF treatment costs 50% more than advertised.
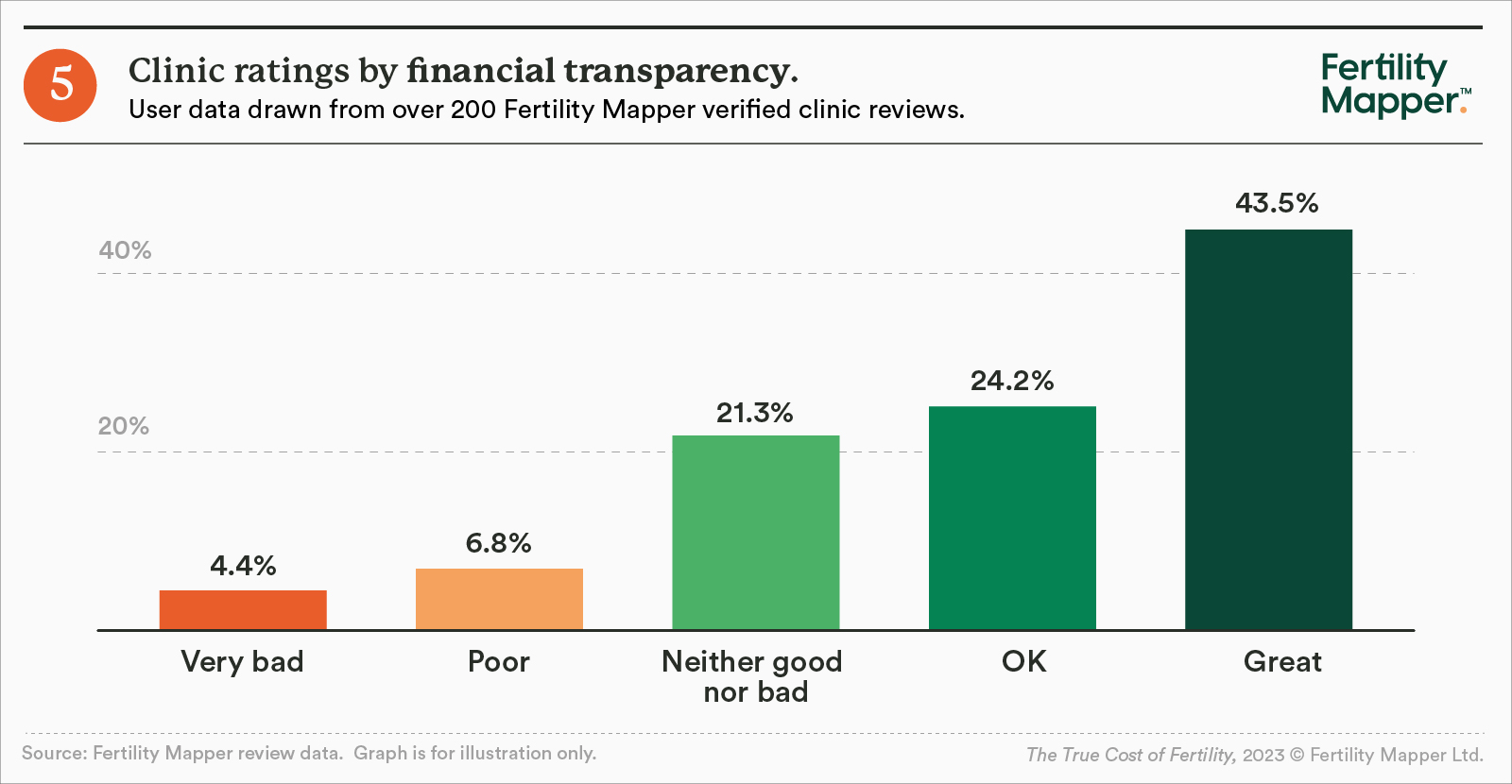
- Data collected from more than 200 reviews on Fertility Mapper's website found that people had major concerns about the financial transparency of clinics:
- One in nine (11%) rated their clinic poorly (0-4 stars out of 10) for financial transparency.
- A third of respondents (32%) said they were not given a fully-costed plan before their treatment started.
- One in six (16%) patients who changed treatment plan were not made aware of any additional costs before the change occurred.
The Family-Building Revolution
Parenthood is a changing landscape, and growing numbers of people need treatment or support from fertility clinics.
Globally, it's estimated that one in six people experience infertility in their lifetime. This is partly age-related, with the average age of mothers rising significantly in recent decades - particularly in the Western world. In the past 40 years in the UK, ONS data shows that the average age of women at childbirth has gone up from 27 to 31.
Meanwhile, research is shedding light on the way environmental factors, such as pollutants, chemical exposure and lifestyle factors, may also impact fertility in men and women.
We are also seeing an important societal shift that moves beyond heteronormative, nuclear family types - such as single parents and LGBT+ families, who may opt to use assisted reproductive technology to have children. HFEA data shows that same-sex female couples accounted for 6.8% of IVF or Donor Insemination (DI) treatments in the UK in 2021, and single women were 7.9%, up from 6.1% in 2019.
As a result, between 2019 and 2021, the number of IVF cycles increased by 9% and DI increased by 22%.
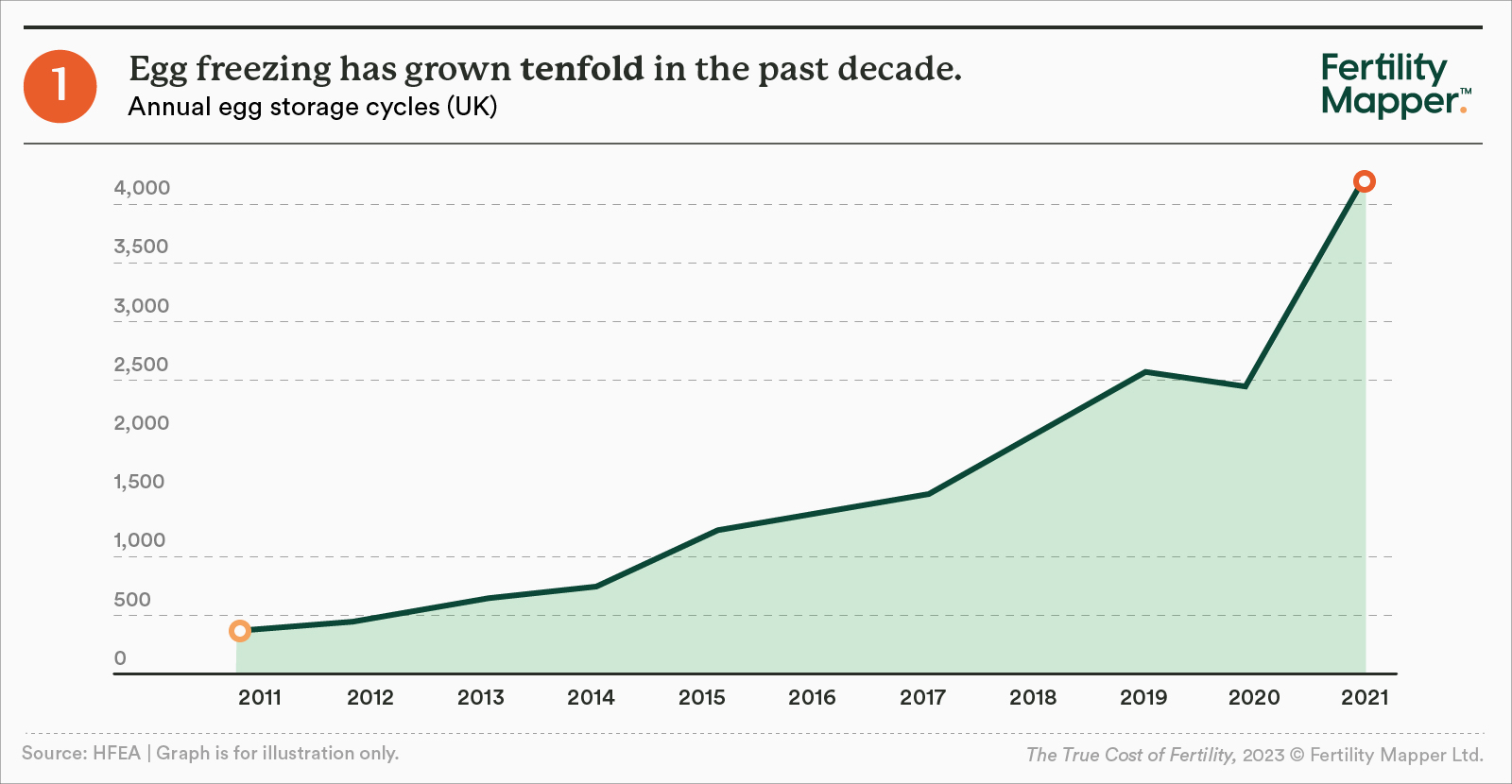
Not only are more people making families, there are also people looking to preserve their fertility, as they look for more time to make their family-building decisions. As a result, fertility preservation treatments have become the fastest growing segment of the market, and egg storage cycles have grown more than tenfold in the past decade. Embryo storage has grown almost fifty-fold. The pandemic turbo-charged this trend: the number of egg storage cycles increased by 64% between 2019 and 2021.
The law now permits storage of eggs, sperm, or embryos for use in treatment for any period up to a maximum of 55 years, providing patients renew consent every 10 years. This means that people now have more time to make important decisions about their future.
These shifts are driving never-before-seen demand for fertility services across the globe. It's estimated that over 12 million babies have been born in the 45 years since the first IVF birth, and today a baby is born by IVF every minute globally.
In the UK, regardless of whether people seek treatment via the NHS or through the private sector, they will face a widespread issue: lack of transparency. Information is often hard to find, frequently confusing and contradictory.
That means that amidst unprecedented demand and need, the fertility sector is failing people as complexity sows confusion amongst the already vulnerable. In turn, this enables the NHS to discreetly cut access to treatment and support, and some private providers to charge much more than their competitors - safe in the knowledge that customers don't see the full playing field.
Until now.
Falling through the NHS net
When it comes to fertility treatment, the NHS is far from equal. Funding for services is determined at a local level - resulting in significant differences across the country.
Fertility Mapper's analysis looked at two key criteria:
- Eligibility - the rules determining who can (and can't) access fertility treatment on the NHS.
- Generosity - the fullness of the treatment on offer within an NHS region.
On Eligibility
The first step people face when accessing treatment is "proving" infertility. While most integrated care boards (ICBs) require at least two years of unsuccessful unprotected sex before being eligible for NHS-funded IVF treatment, six (16%) require three years of trying. The reality is, when this is combined with long waiting lists for treatment (many being a year or more), people lose precious time - a critical problem when age is considered a leading factor in infertility.
Meanwhile, half of England's ICBs require female same-sex couples to have undergone at least 12 cycles of failed artificial insemination before being eligible for IVF - and almost all require those 12 cycles to be self-funded. The average price of a round of IUI at a private clinic is £1,265 excluding donor sperm, so many couples incur considerable cost before being considered for NHS-funded IVF.
Other factors further add to the complexity:
- In almost a fifth of ICBs (19%), people cannot have accessed IVF previously - even if it was self-funded privately.
- Almost half (46%) of regional NHS boards in England will only offer IVF if the maternal partner is aged under 40 - and one ICB will only offer IVF if she is under 35.
- All ICBs impose a BMI maximum limit on the maternal partner, and more than a third also impose a BMI maximum on the paternal partner.
- Three-quarters (76%) of ICBs will only fund IVF if neither partner has any living children, while others allow it if the children are from previous relationships.
- One in six of England's ICBs will only fund IVF if the couple has been together for at least two years.
In reality, eligibility is not just a postcode lottery based on where you live - it's also a personal lottery.
On Generosity
Once eligibility criteria have been met, people may discover that NHS fertility services in their local area are more limited than they expected.
Nearly three-quarters of ICBs, for example, will only fund one cycle of IVF. After treatment, 40% of ICBs will only store surplus embryos for free for one year.
The wider impact
In practice, what this means is that large numbers of people don't qualify for NHS-funded fertility treatment, and if they do, they may find that their options for treatment are limited. Similarly, while some will qualify for the NHS at first, given IVF's first-time success rate is 25-30%, many people may need to continue treatment beyond what the NHS offers.
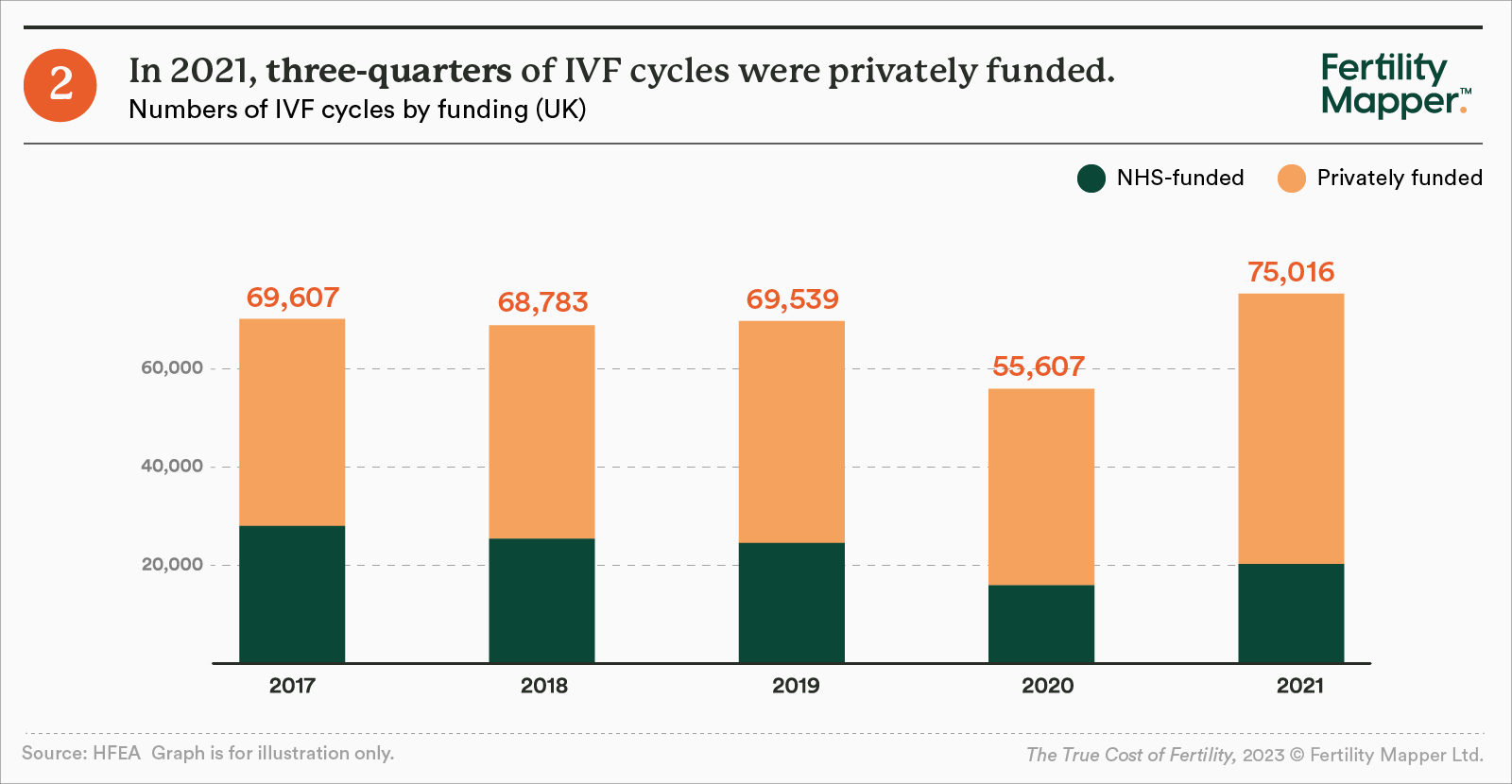
It is perhaps unsurprising, then, that the proportion of fertility treatments that are funded by the NHS has fallen significantly in recent years. In 2021, just 27% of IVF cycles were funded by the NHS, compared to 40% in 2017.
For many, it's not only the fact that they can't access NHS-funded fertility services (which, besides being free, also carries with it familiarity and an expectation of wider support). It's also the toll of navigating the additional complexity of the system at a time of immense personal stress, causing immense frustration. For some, the sheer lack of transparency means they may wait years for treatment - only to discover they're not eligible under the NHS. With age a key fertility factor, these years could be the difference between a successful conception, or not.
Our Stories: Laura & Jack
When Laura's first round of IVF failed, it was only by picking through the fine print of her local care commissioning group's (CCG) terms and conditions that she found out she was eligible for another round. But she feels frustrated at how much self-advocacy it took to get the service she was entitled to.
"It's almost as if, like, if you want to make it work, you have to go and do the research as if you were a doctor," she says. "They don't consider you as an individual."
Although the second transfer didn't work, Laura and Jack do have two frozen embryos left, so they are now waiting until they are financially and emotionally ready to move to privately-funded treatment.
"It's definitely derailed our life plans because we've got to put those finances aside, so we do feel stunted at the moment," she says. "I'd be lying if I said it doesn't take over your life because it does even now. We've been on a break, but I've never stopped thinking about it."
Navigating the private sector
Everyone entering the private fertility market comes from different entry-points. Some may want a treatment which isn't available on the NHS; some may not be eligible, while others may choose to go privately due to the long waiting times. Others, meanwhile, have already been through NHS-funded options, but weren't successful.
A common factor, however, among those starting private treatment is that this is likely to be the first time they have paid for healthcare services. A reality which, in the UK, is a new and daunting experience.
Healthcare services, including fertility treatments, are expensive. They're inherently complex to buy. There's a huge number of clinics all offering packages at different price points, with different levels of coverage available. Until now, there was no comprehensive source to help people distil the good from the bad. This leaves "patients" - now also customers - to make one of the most costly and complex decisions of their lives at a time when they are also vulnerable and frequently underprepared.
Fertility Mapper analysed 100 private clinics across the UK using a standardised methodology, along with itemised price lists from each clinic, to estimate how much an average "true standard" treatment would really cost. Our analysis assessed costs across:
- Pre-treatment
- Treatment
- Common extras
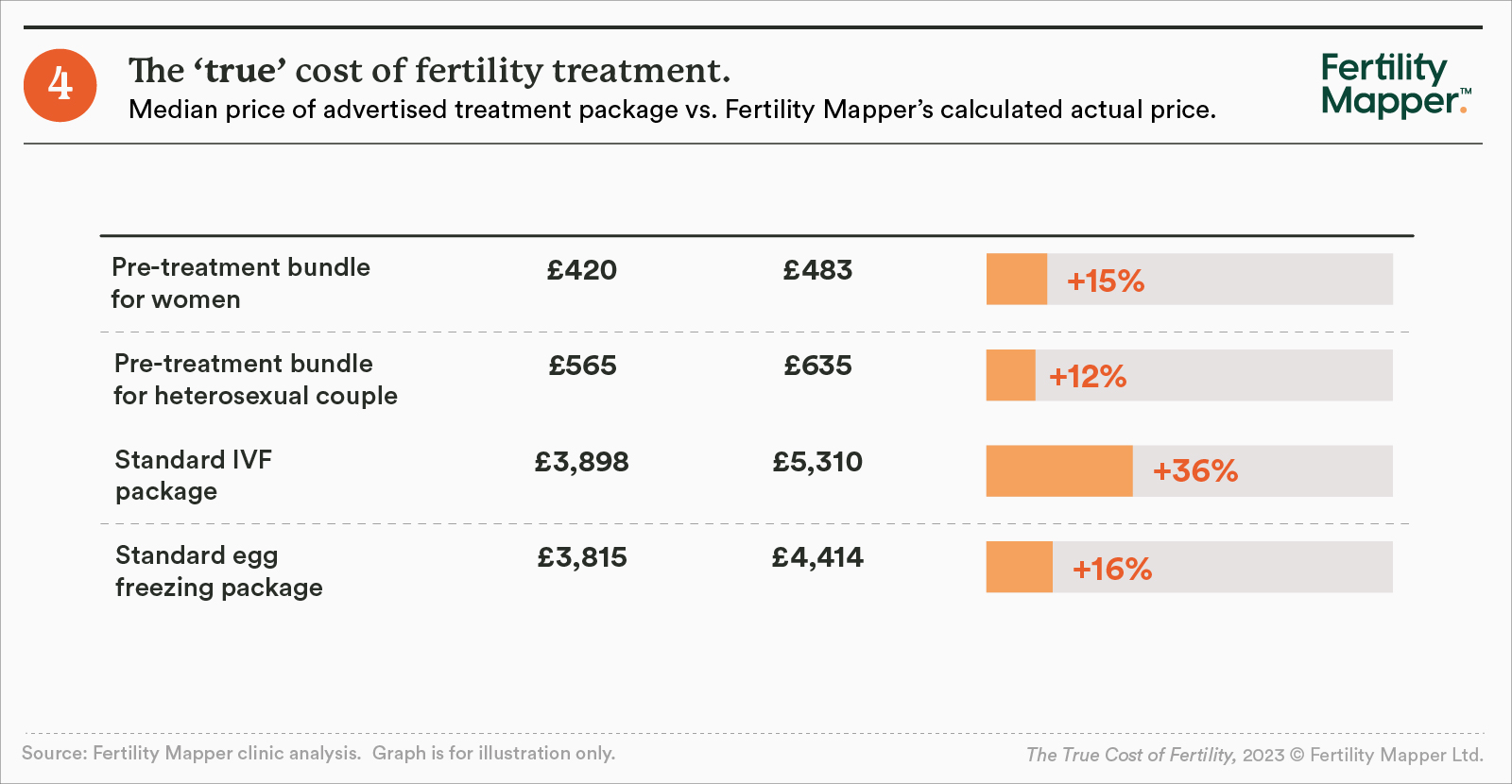
The results revealed huge variation in what is offered in advertised treatment "packages". In a large number of cases, the price of a true standard fertility treatment may end up being much higher than expected.
And importantly, some clinics that appear the most cost-effective can become the most expensive - with thousands of hidden costs potentially added to the final bill. On the other hand, clinics that seem more expensive at a first glance may in fact be more transparent in their pricing. For many people, though, telling the difference is almost impossible.
Our Stories: Frank
Frank and his partner's twin boys were born through IVF with ICSI, a treatment they funded privately through family support. Despite being shown a price list at the beginning of their treatment, and being quoted a "ballpark" figure of around £9,000, their treatment ended up costing around £13,000 due to extra costs, particularly medication. But by that point they'd already committed to the clinic with their pre-treatment tests, so didn't feel like they could change.
"If they'd just said from the beginning how much it would be we would have been prepared, but it was so much more than they'd said," he says. "Taking money from family for fertility treatment is weird enough as is, having to ask for more creates such a strange dynamic."
"It was really worrying and stressful, and added so much pressure for the pregnancy to be successful. But you're not going to stop the treatment, so there's nothing you can do."
Pre-treatment
Treatment starts with initial tests and consultations, which is usually packaged up as a "pre-treatment bundle" or "fertility MOT". These bundles cost anywhere from £200 to £650 - but not all bundles include everything needed, such as AMH testing or a thyroid function check. At some clinics, these necessary tests then cost extra.
Our analysis found that while the average pre-treatment bundle for a woman is priced at £420, the true price for all the core treatments needed, including a thyroid function check, averages £483. That's 15% higher than advertised. Meanwhile, the average price for a pre-treatment bundle for a heterosexual couple is £565, but Fertility Mapper calculates the true cost is £635 - 12% more.
This is only the beginning, but for many at this point, they have committed to a clinic. Moving to a new one is likely to mean starting the process all over again - and paying for more consultations and tests.
Treatment
Common extras
Finally, there are also common extras - or "add-ons" - which many people opt for. These vary a lot in price. ICSI, which is used in 49% of IVF cycles, can cost anywhere from £800 to £1675, with the median sitting at £1,300. Meanwhile, an additional year of embryo storage can cost anything between £175 and £440.
One key area our analysis didn't deep-dive into is the cost of medication. Here, though, people might be quoted anywhere from £250 to £3,000 - with the exact amount differing significantly from person-to-person.
Just one in 10 of the clinics we analysed includes medication in their standard package - instead, most sell medication separately and at a significant mark-up. Individuals do have the choice to purchase medication at an independent pharmacy, but may not be aware of this option. And, in some cases, a prescription to take elsewhere may cost hundreds of pounds.
It's not all about the money
The issue isn't the range in prices - it's up to the clinics how they want to price services, and up to customers how much they choose to pay. The real issue is the lack of financial transparency, which means that at some clinics, customers face bills of thousands more than expected. All while they're undergoing the emotional and physical toll of treatment. It also makes it impossible for customers to pick a clinic based on price.
At Fertility Mapper, we see the impact of this lack of transparency in the personal reviews left on our site. Analysis of hundreds of reviews found that although four in ten respondents ranked their clinic very highly for financial transparency, there was a significant proportion who did not feel happy with the information they received.
- One in nine (11%) ranked their clinic between zero and four (out of 10) in terms of financial transparency.
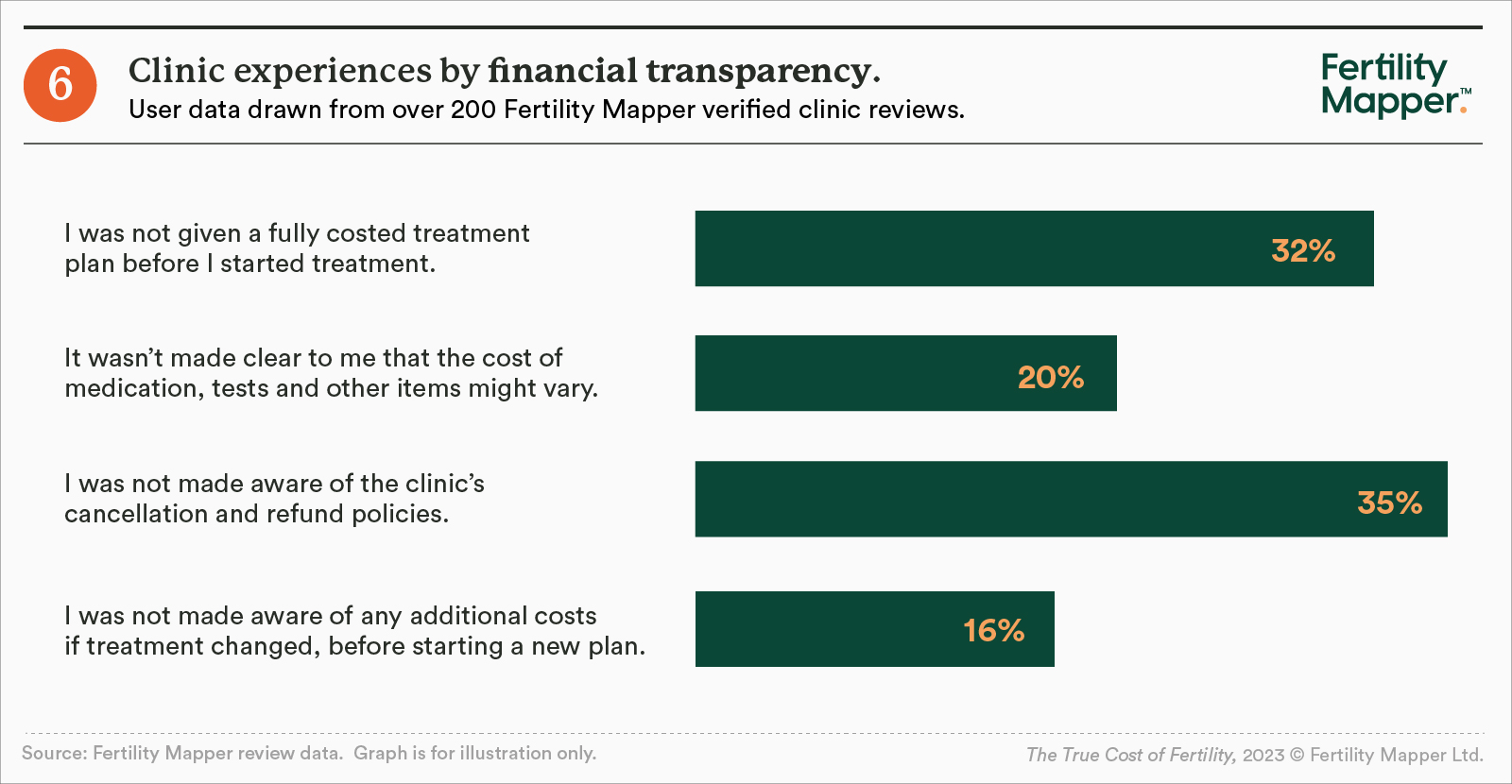
- Almost a third (32%) of respondents said they were not given a fully-costed plan before their treatment started, and a third said they weren't told about cancellation and refund policies.
- Of more than 90 respondents who changed treatment plans, one in six (16%) said they weren't made aware of any additional costs of the new plan.
Where do we go from here?
The True Cost of Fertility report highlights that more needs to be done to make access to fertility treatment less overwhelming and confusing for people, however it's funded.
The data paints a clear picture of a sector where bad practice can easily hide, as is the case around the lack of financial transparency some private clinics show. It also throws into stark relief the extent to which people are forced to navigate poor information across both the NHS and the private market at a vulnerable time in life.
The report's most important takeaway, however, is that the key antidote to all this complexity is greater transparency. Transparency can equip people with information they need to manage their money, plan, and make the best choices for them. That is the core driver behind this report.
At Fertility Mapper, there are two key ways that we're focused on improving transparency today and making a tangible difference for people:
- NHS IVF Eligibility Calculator - users can access, for free, Fertility Mapper's unique calculator, which enables people to quickly and easily assess their personal eligibility for NHS-funded treatment.
- Clinic Search - users can search, for free, fertility clinics pages containing pricing information and community reviews, complete with detailed scores and personal feedback, to help them pick the best clinic for them.
Community fight-back
We also believe it's time for the fertility community - those who have previously undergone, or are currently undergoing, treatment - to raise their voices and share their stories.
At Fertility Mapper, we have created an anonymous space for individual stories and experiences, as well as ensuring we share accurate, transparent review data. But this is not enough. To drive change, the community needs you - the thousands of individuals who have been through treatment - to provide your feedback on clinics.
Because while an individual may not have the same power as a government or an insurance company to negotiate prices and set standards in a private healthcare market like fertility, we do have collective power. The power to become an informed, active consumer group demanding better for both ourselves, and those who come after.
About Fertility Mapper
Fertility Mapper is a platform powered by community data, dedicated to improving personalised access to high quality fertility services. We're fundamentally rethinking the way fertility treatments are experienced, delivered and paid for.
Today, that involves setting a new standard for transparency in the sector. Think of us as Tripadvisor for fertility clinics: a community-powered one-stop shop for anyone accessing treatment. By combining verified clinic reviews with expert information, our goal is to empower people to make informed choices - putting them firmly in the driving seat. The data from our reviews also provides clinics with a vital and much-needed feedback loop - improving performance and service quality, and opening new opportunities for innovation.
Coupled with its NHS IVF eligibility calculator, which helps people quickly understand NHS eligibility criteria relevant to them, Fertility Mapper aims to help people navigate the complex world of assisted fertility - whether that includes the NHS, the private sector, or both.
And we're just getting started.
Contact Information
For further information about this report, please contact hello@fertilitymapper.com.



